AR Calling (Denial Management) in Medical Billing RCM
"Job-Ready Skills for AR Calling and Denial Management in U.S. Revenue Cycle"
4.51 (42 reviews)

465
students
2 hours
content
May 2025
last update
FREE
regular price
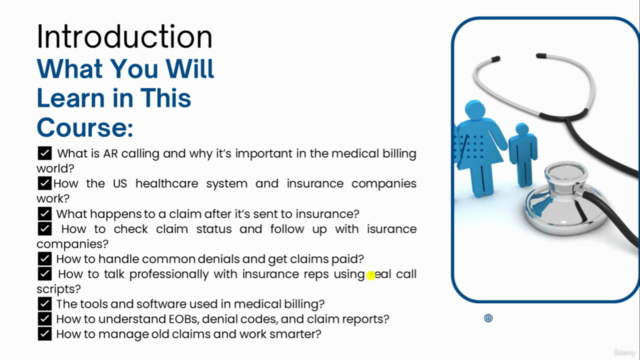
What you will learn
Understand the U.S. healthcare system and insurance terminology, including payer types (Medicare, Medicaid, Commercial, etc.).
Explain the medical billing workflow, including patient registration, charge entry, claim submission, and payment posting.
Perform AR calling professionally, using scripts and soft skills to follow up with insurance companies regarding unpaid or denied claims.
Identify and analyze common claim denials, such as timely filing, medical necessity, coordination of benefits (COB), authorization issues, and more.
Document call outcomes clearly and accurately in the billing system using appropriate follow-up actions.
Develop communication skills to speak confidently with U.S. insurance representatives and explain billing issues to providers or supervisors.
Prepare for job interviews and mock calls as an AR Caller in real-world U.S. healthcare revenue cycle management (RCM) settings
Course Gallery

Loading charts...
6596203
udemy ID
03/05/2025
course created date
08/05/2025
course indexed date
Bot
course submited by